Adult obesity has more than doubled in the last 3 decades8
~890 million adults are living with obesity8
∼5 million premature deaths in 2019 as a result of higher than optimal BMI contributing to noncommunicable diseases8
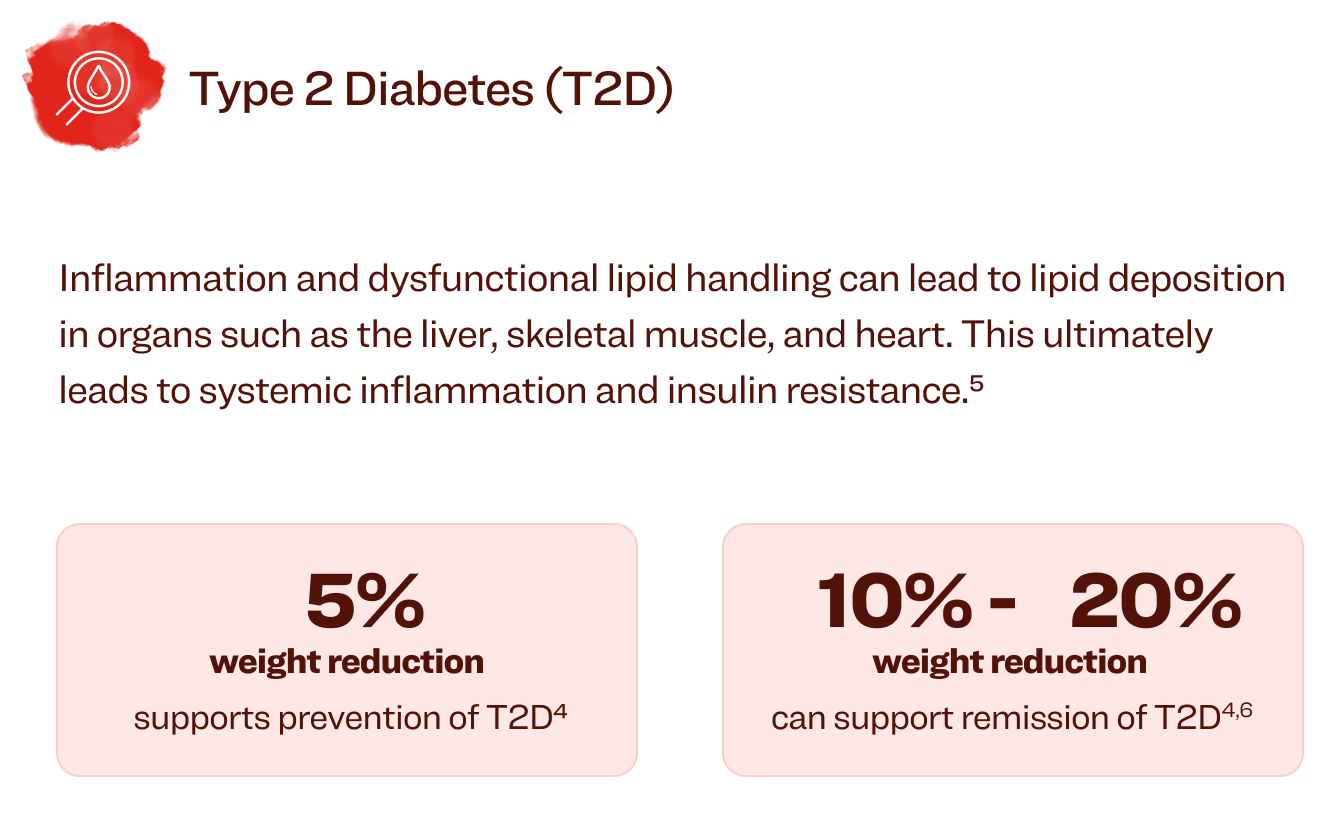
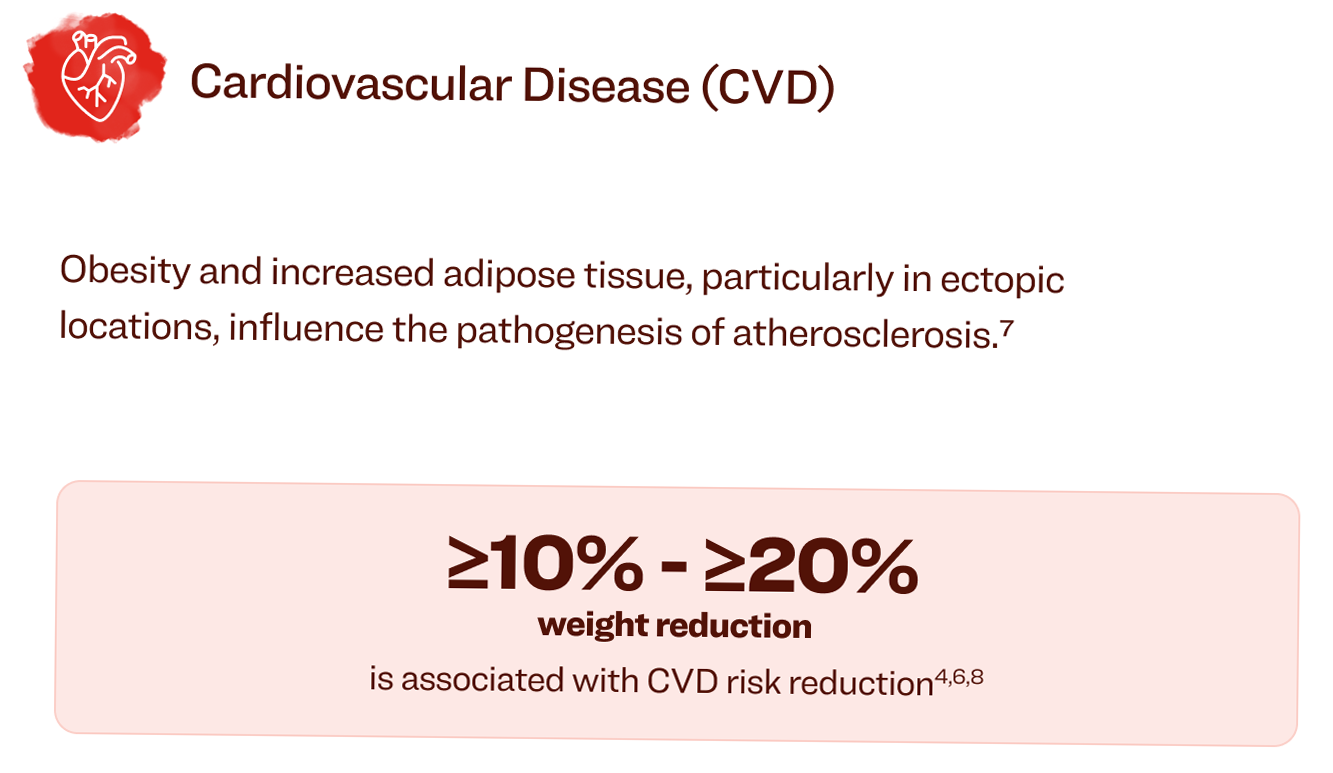
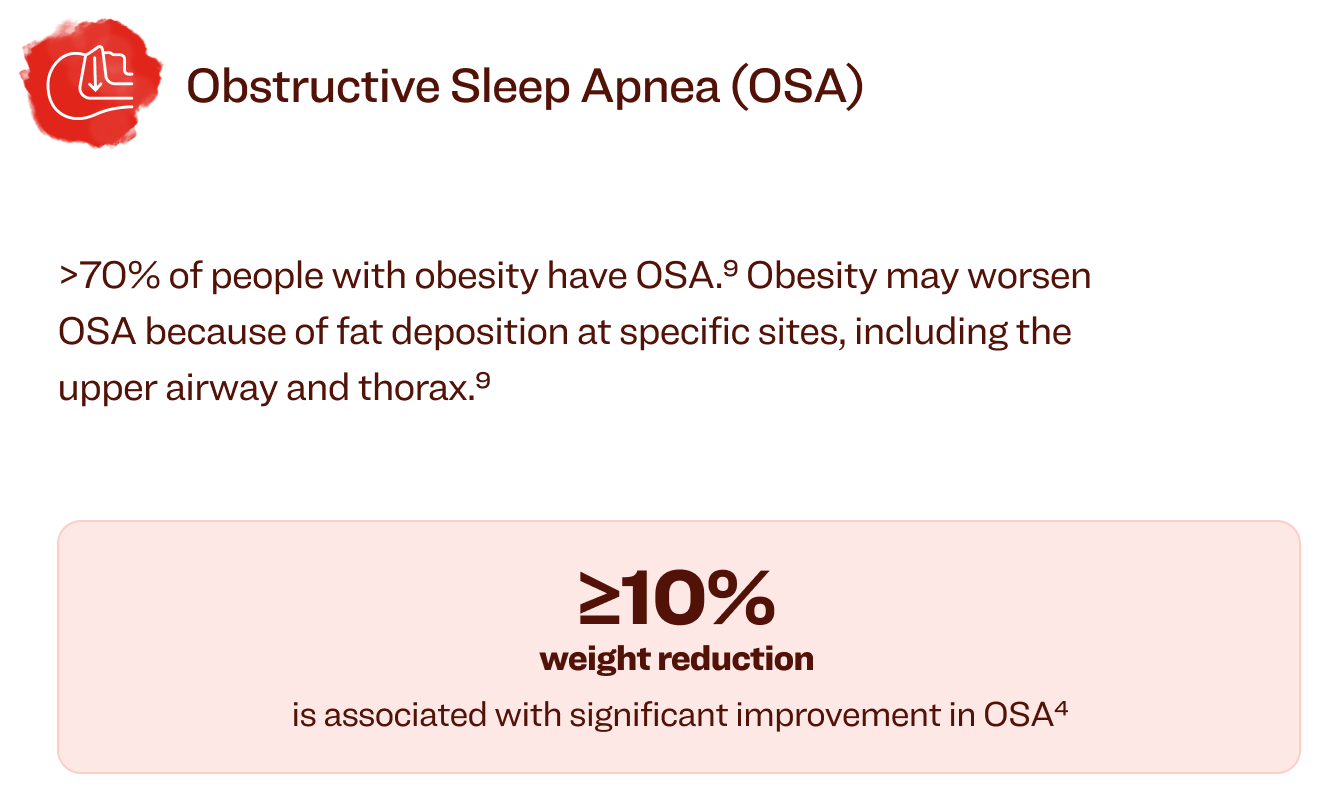
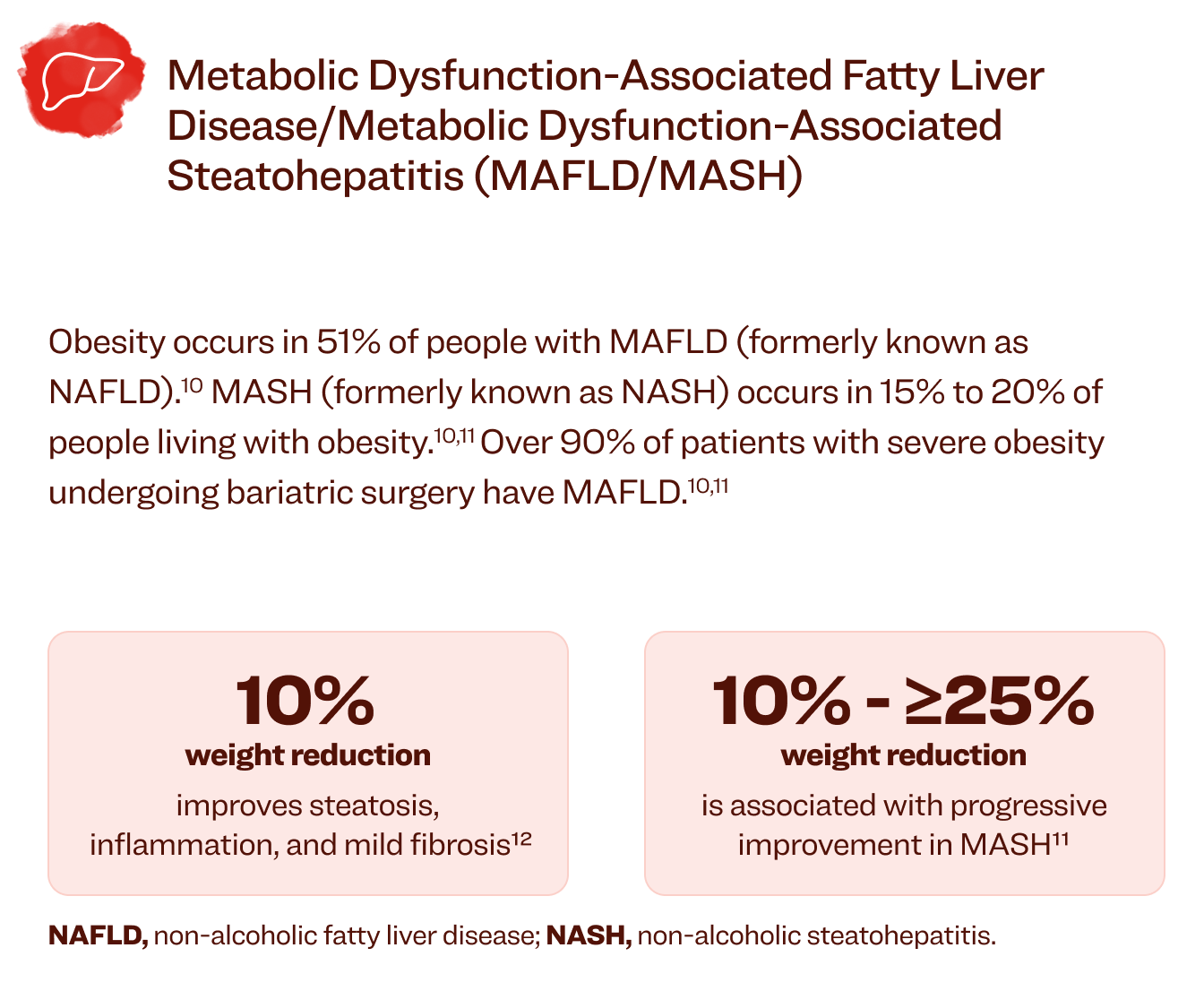
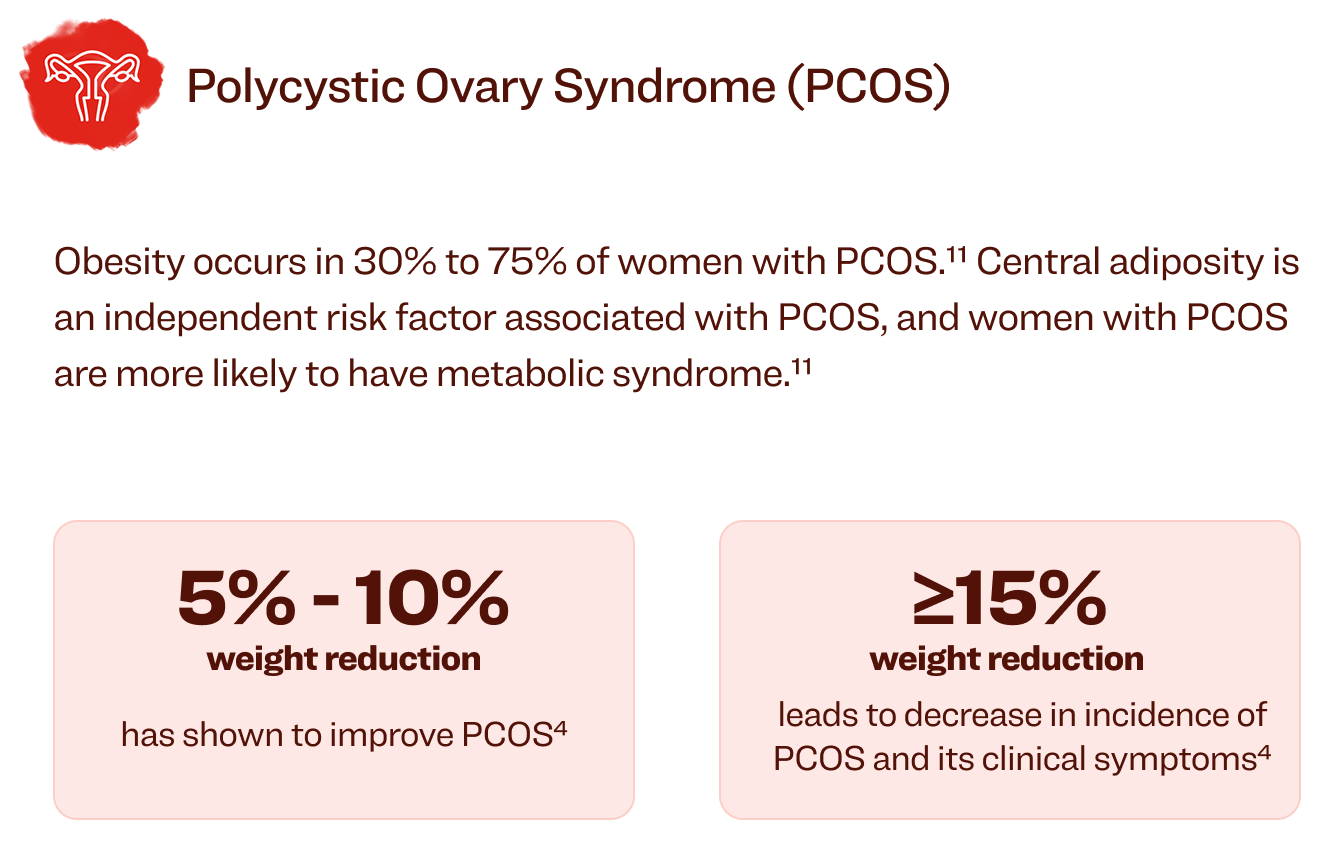
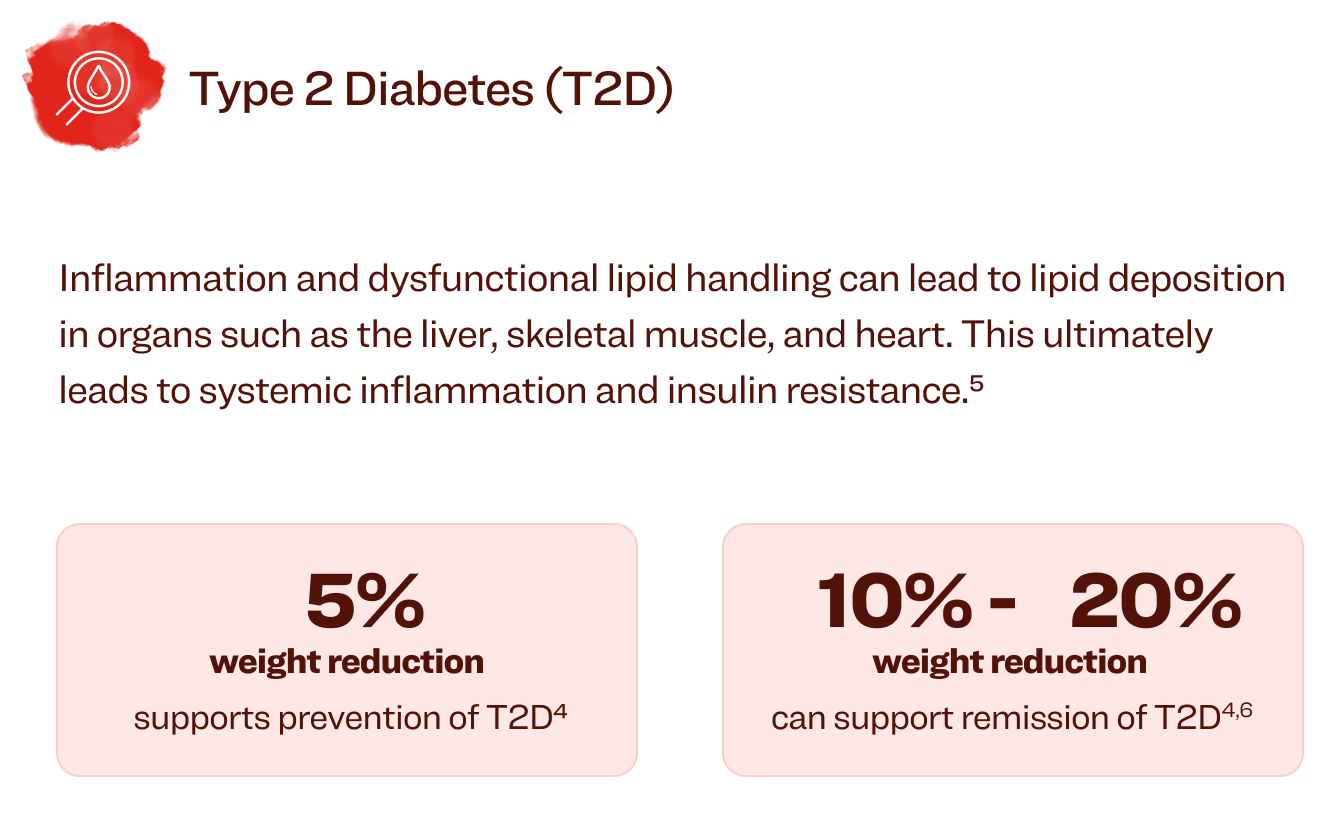
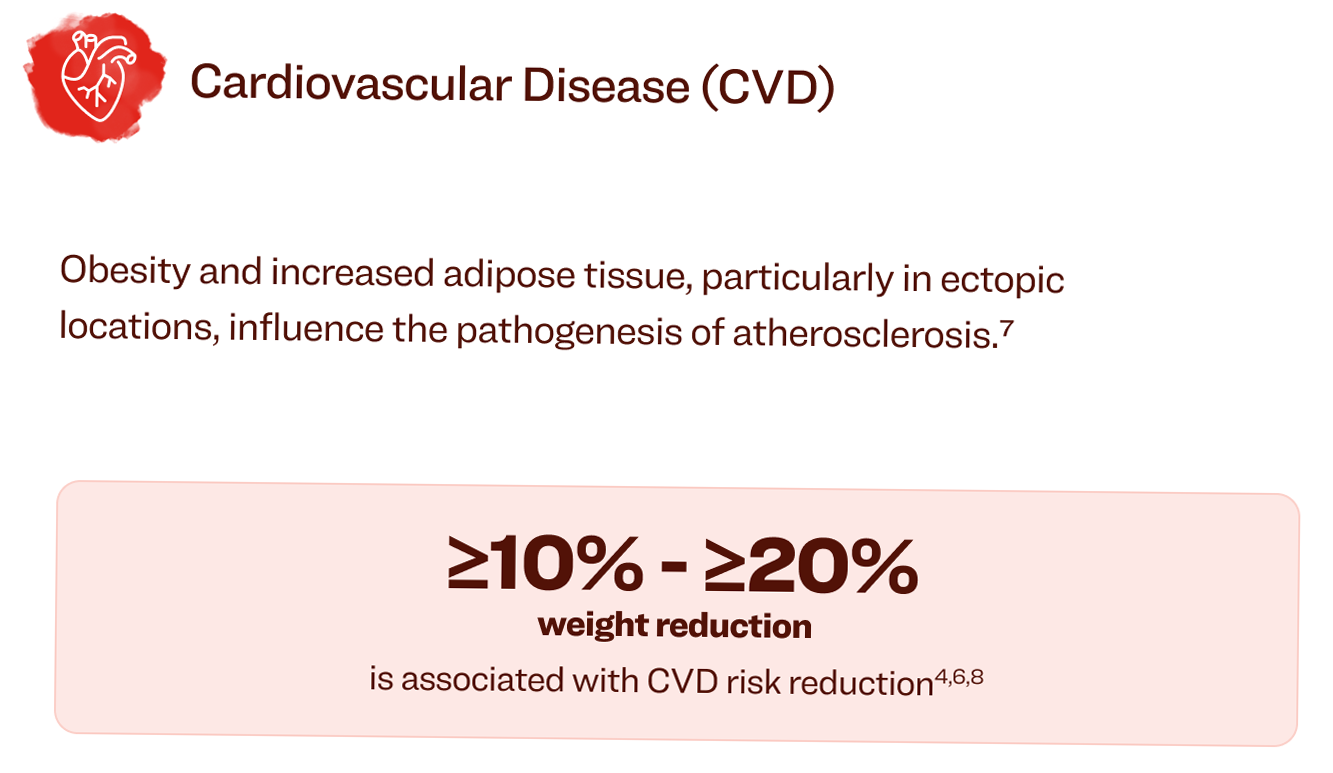
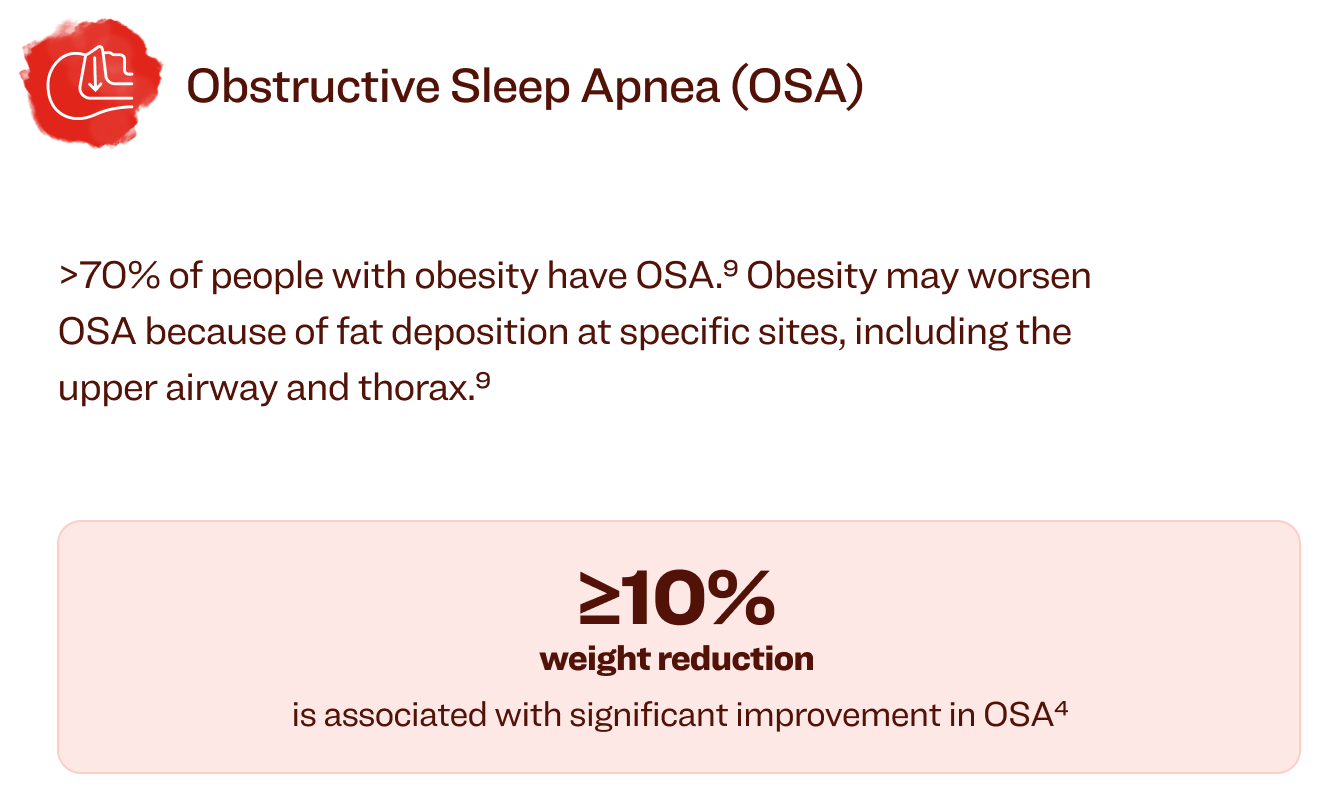
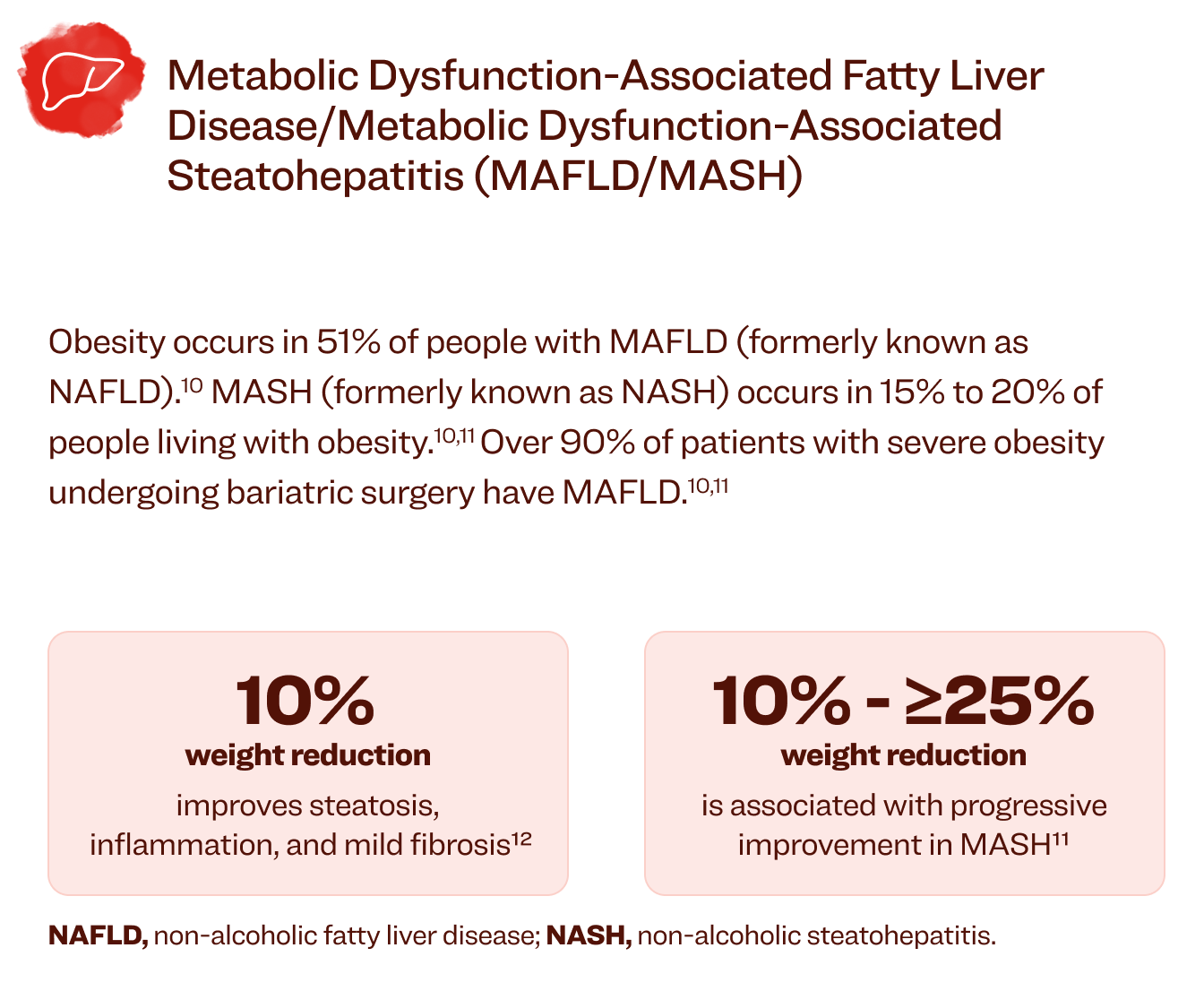
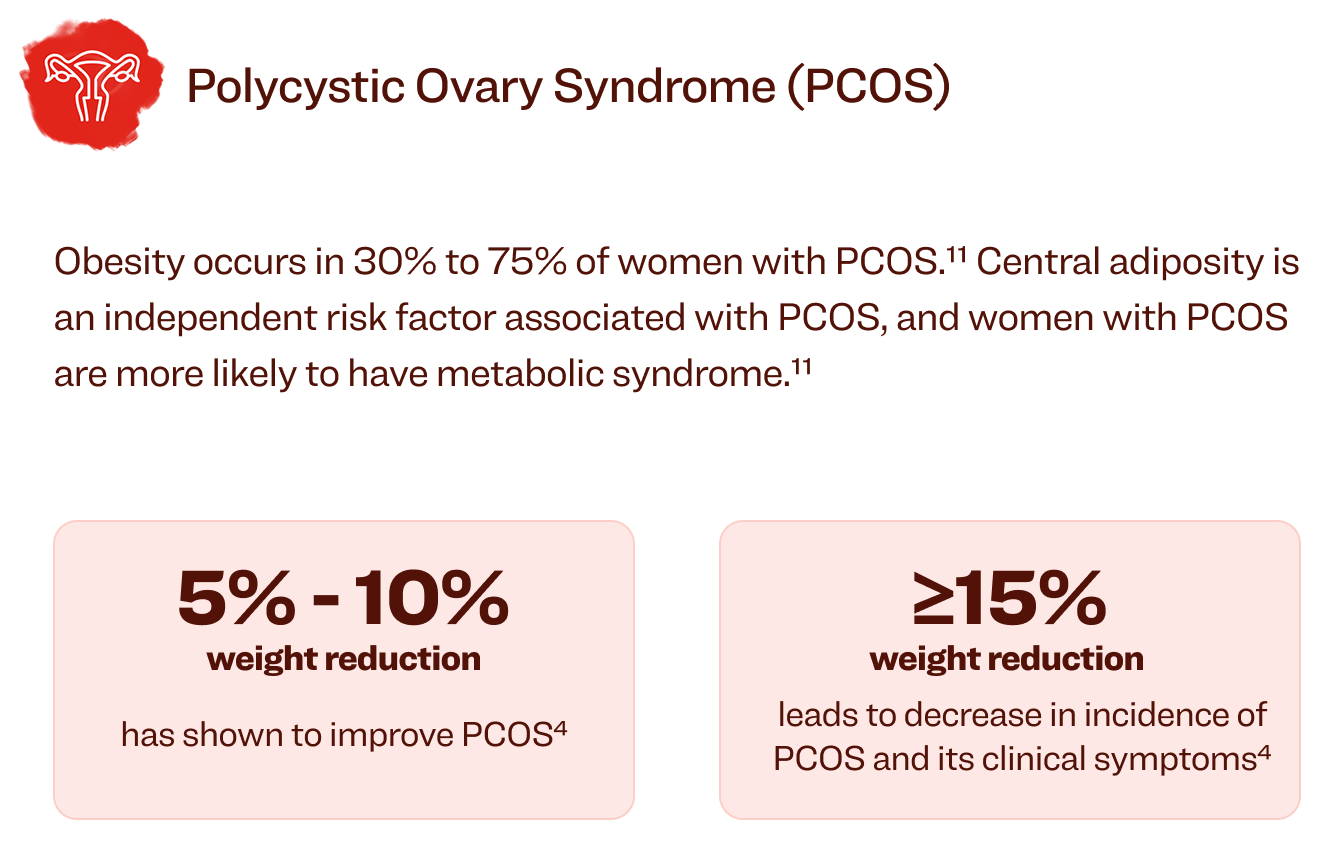
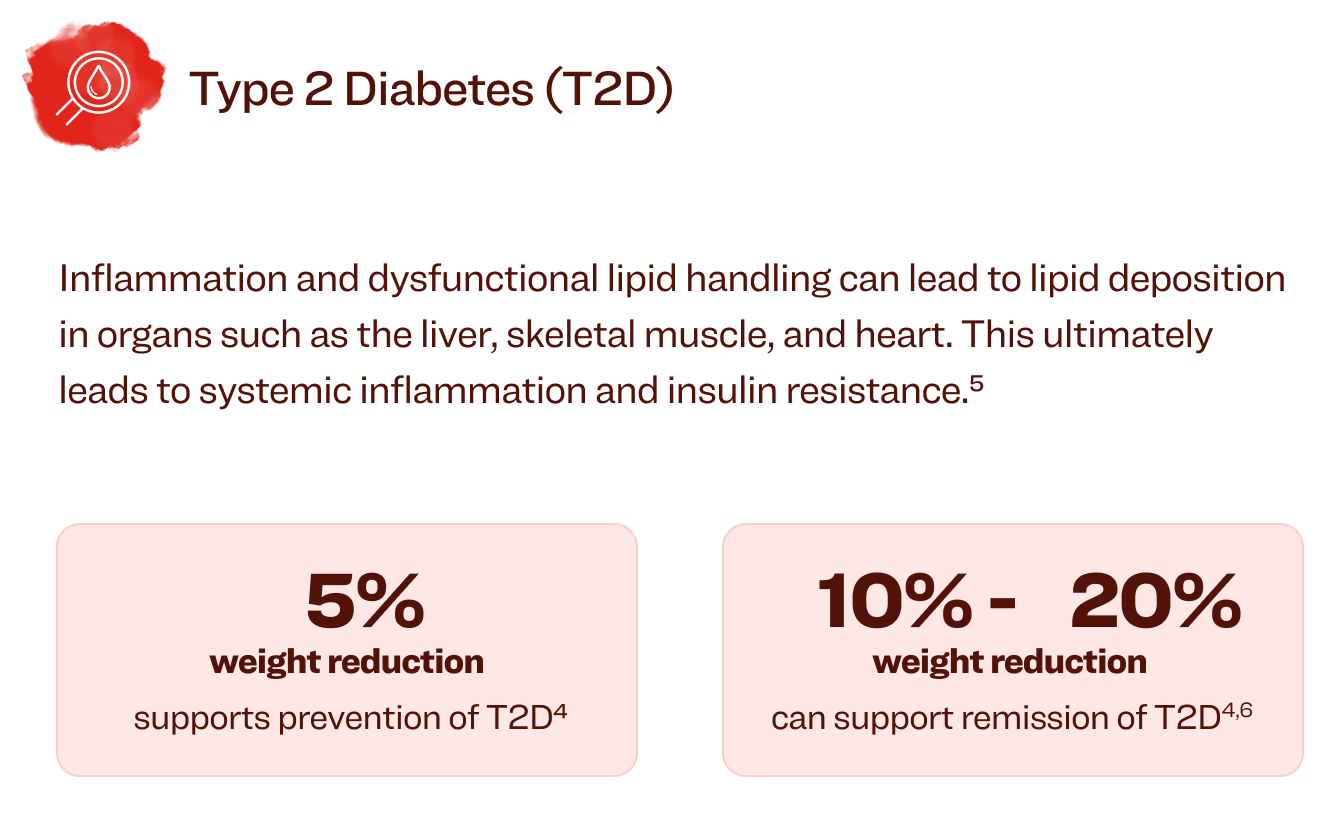
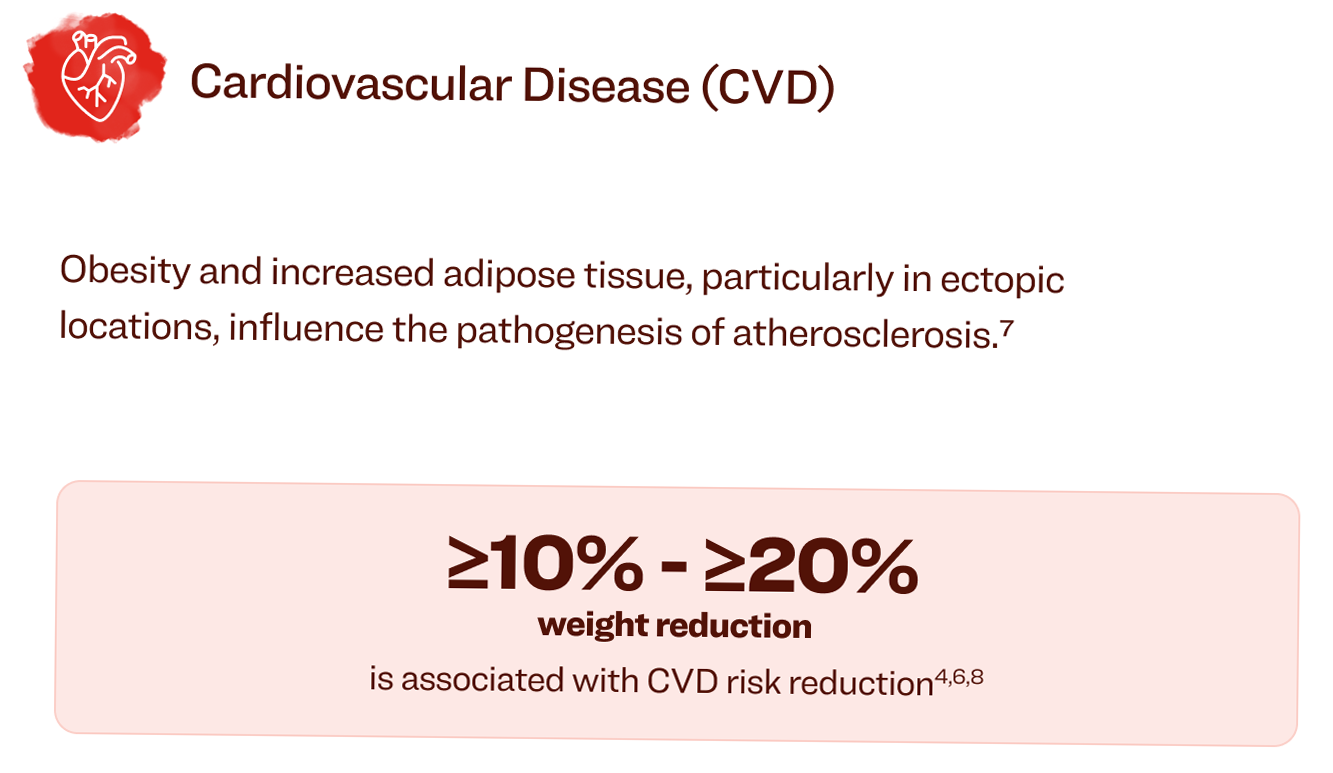
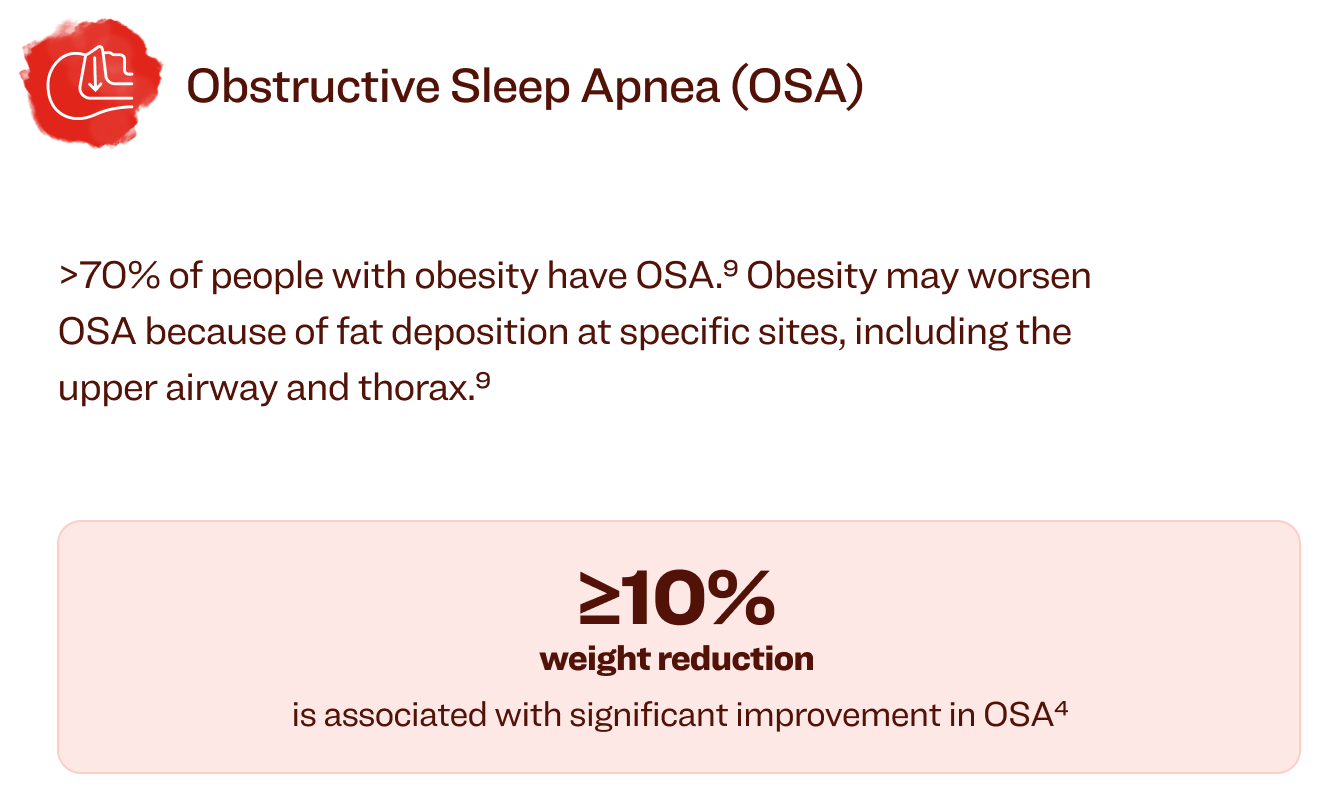
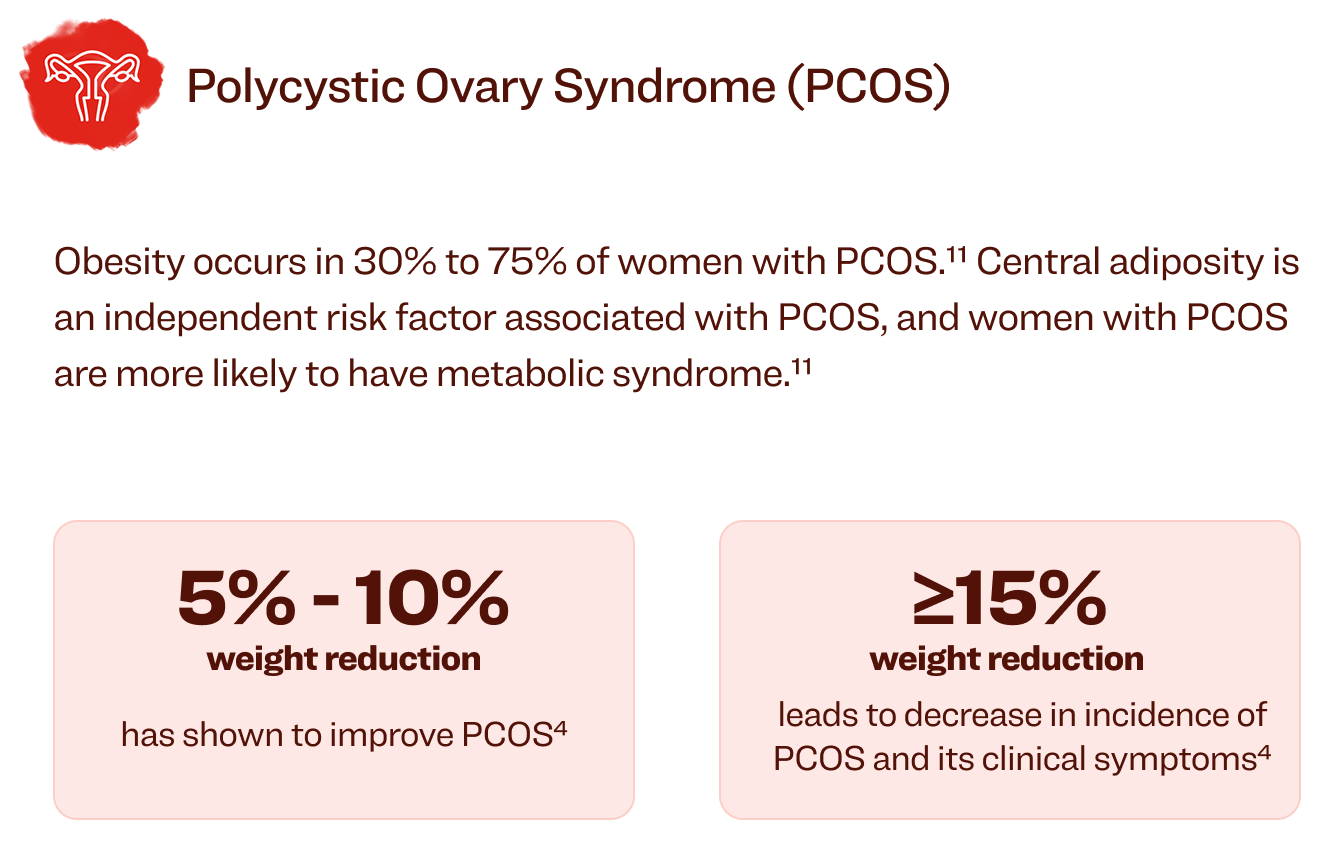
As obesity rates increase, so do the risks of obesity-related complications.9 These include type 2 diabetes, hypertension, coronary artery disease, and several cancers.9 However, weight loss of ≥5% to ≥25% improves many obesity-related complications.3,9,10
We can do more than we think to improve health

BMI, body mass index.
References


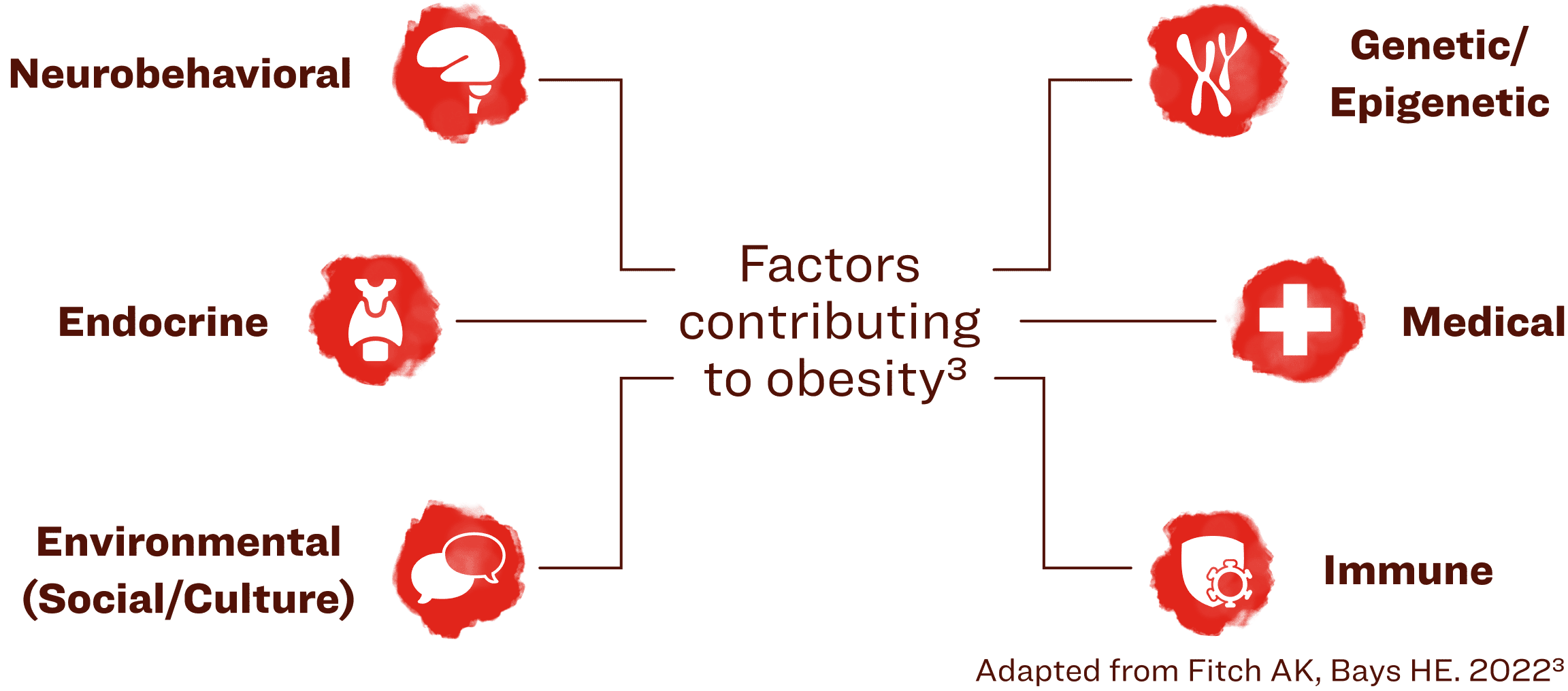
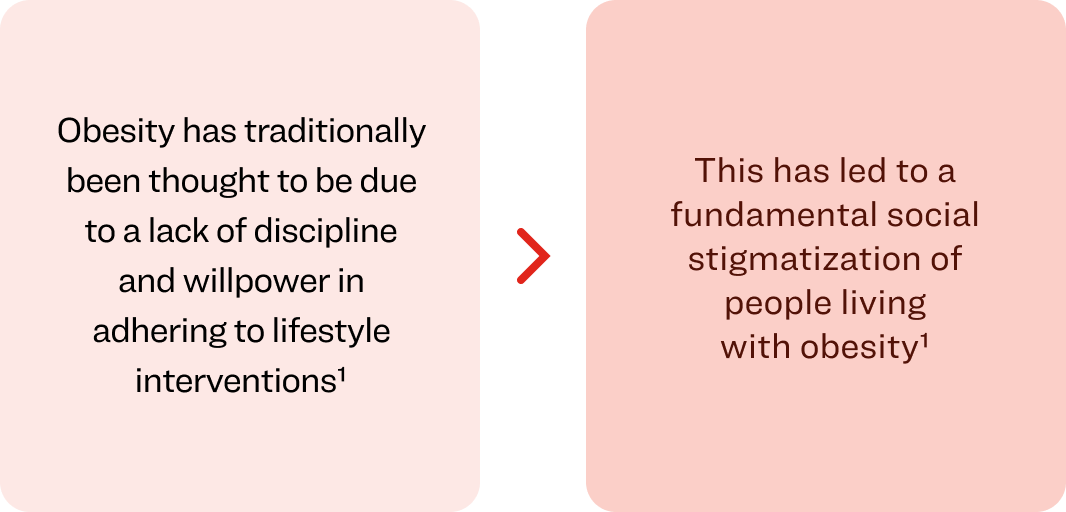
The multifactorial nature of obesity leads to individual variations, requiring a patient-centered, individual approach to management and treatment.3
Obesity is a highly prevalent chronic disease characterized by excessive fat accumulation or distribution that presents a risk to health and requires life-long care. Virtually every system in the body is affected by obesity. Major chronic diseases associated with obesity include diabetes, heart disease, and cancer.4
Adipose tissue has long been misunderstood as just a storage organ for energy. However, with the rise of obesity, adipose tissue is now being recognized as an essential organ in regulating energy homeostasis.6


References
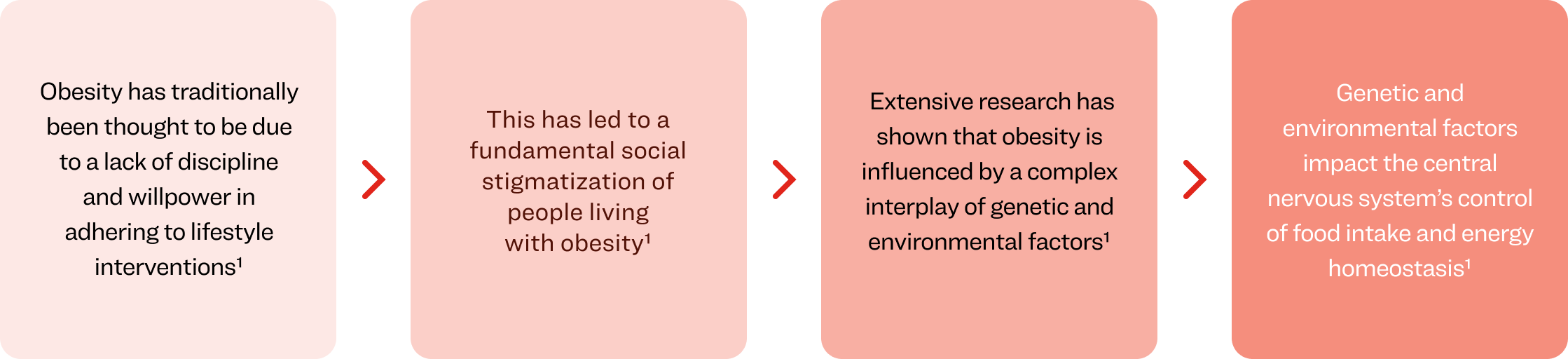
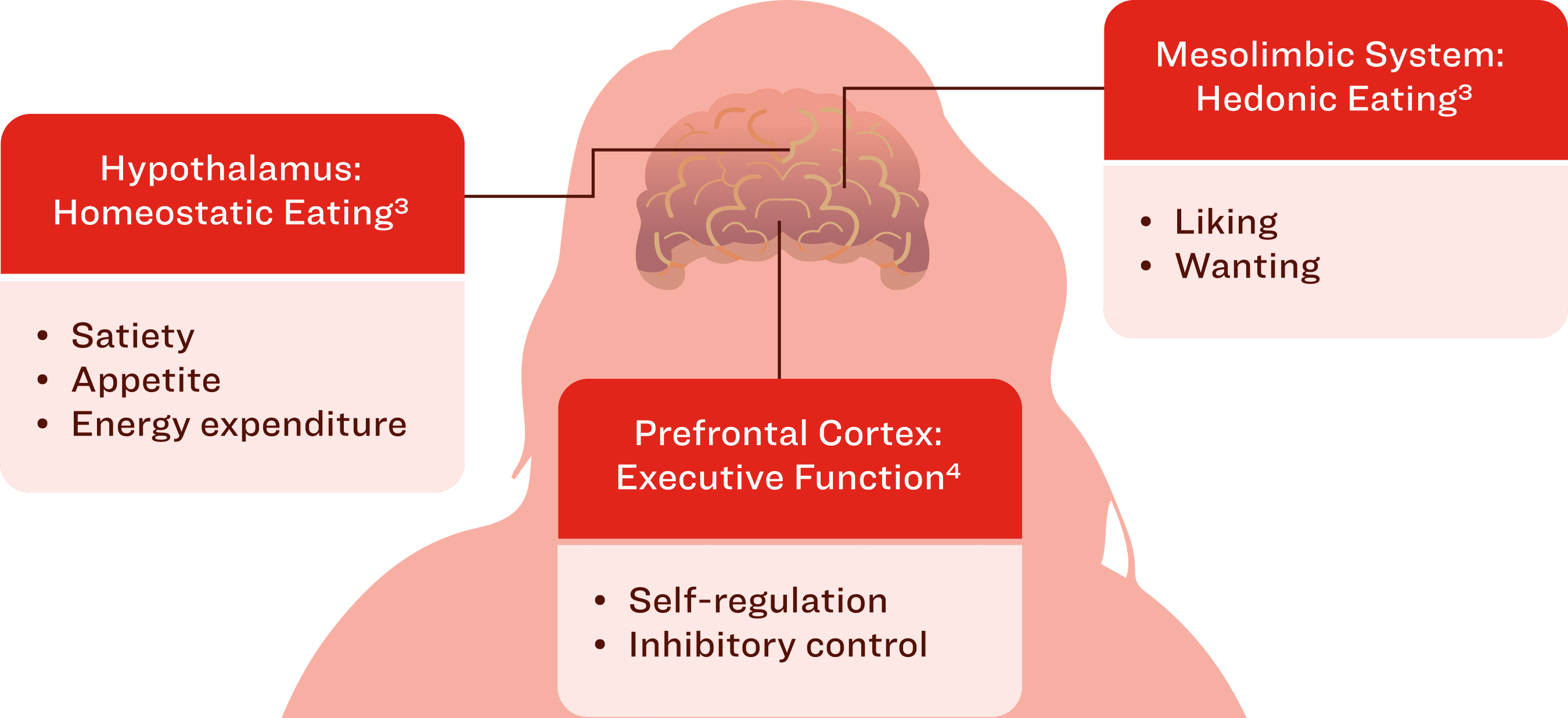
The brain plays a key role in regulating energy balance through its effects on caloric intake and energy expenditure.1

CCK, cholecystokinin; GIP, glucose-dependent insulinotropic polypeptide;
GLP-1, glucagon-like peptide-1; OXM, oxyntomodulin; PYY, peptide YY.

Many of the hormones, peptides, and nutrients involved in the homeostatic regulation of body weight are perturbed after weight loss, and many of these alterations persist for 12 months after weight loss.7
These alterations also persist after weight regain, highlighting a strong physiological basis for the relapsing nature of obesity, and not simply the result of voluntary resumptions of old habits.7

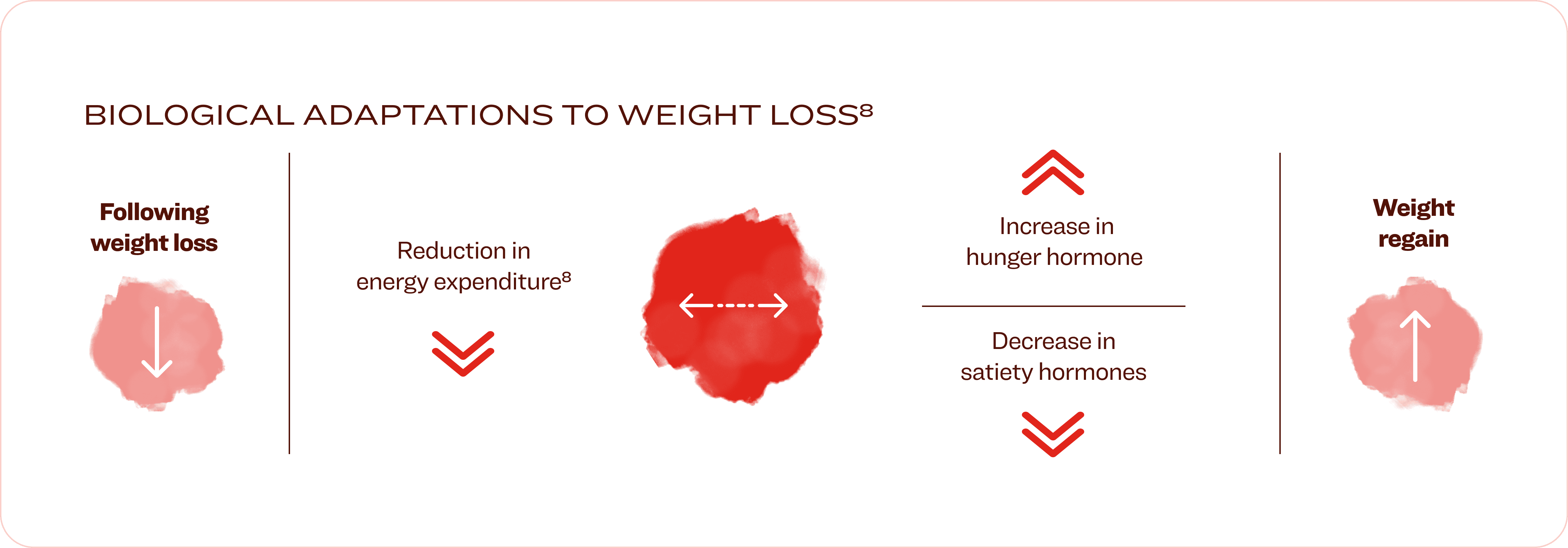
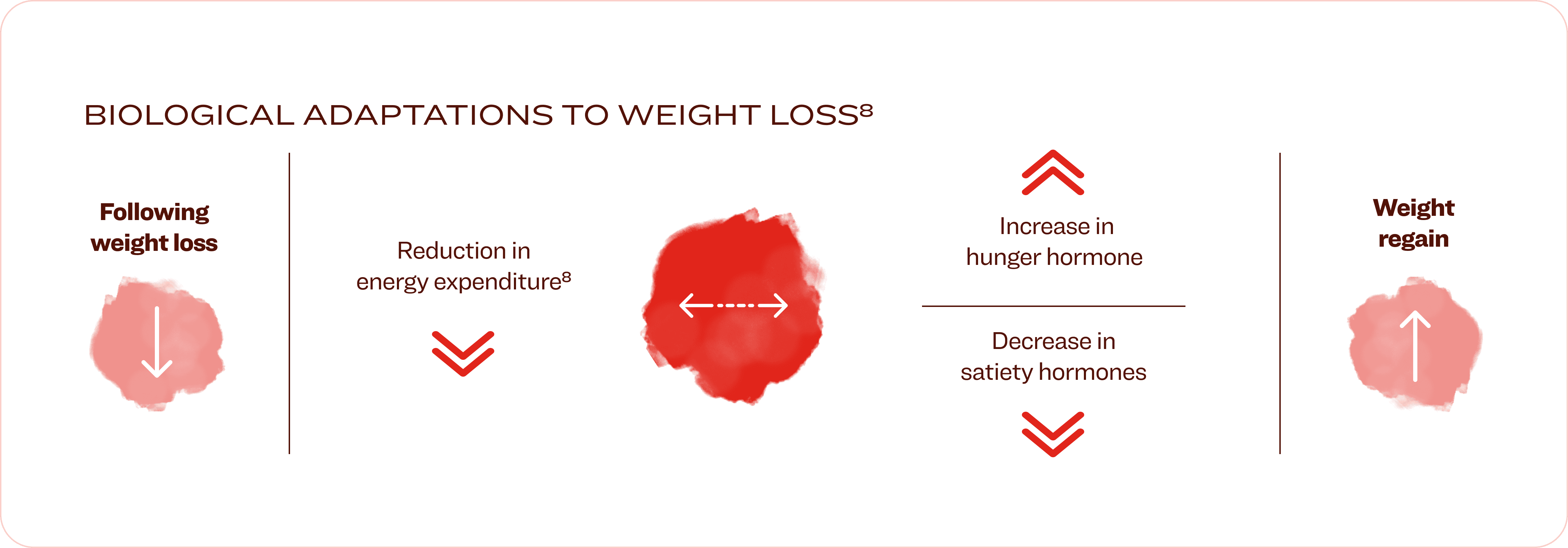

There is a widespread assumption that diet and exercise can entirely reverse obesity over long periods of time.
This belief contradicts the indisputable scientific evidence demonstrating that voluntary efforts to reduce body weight activate biologic responses
(e.g., increased appetite and decreased metabolic rate) that typically promote long-term weight regain.11
References

In 2019, higher than optimal BMI caused an estimated 5 million deaths from noncommunicable diseases.2
Obesity can affect almost all organ systems and is associated with over 200 complications.1,3,4
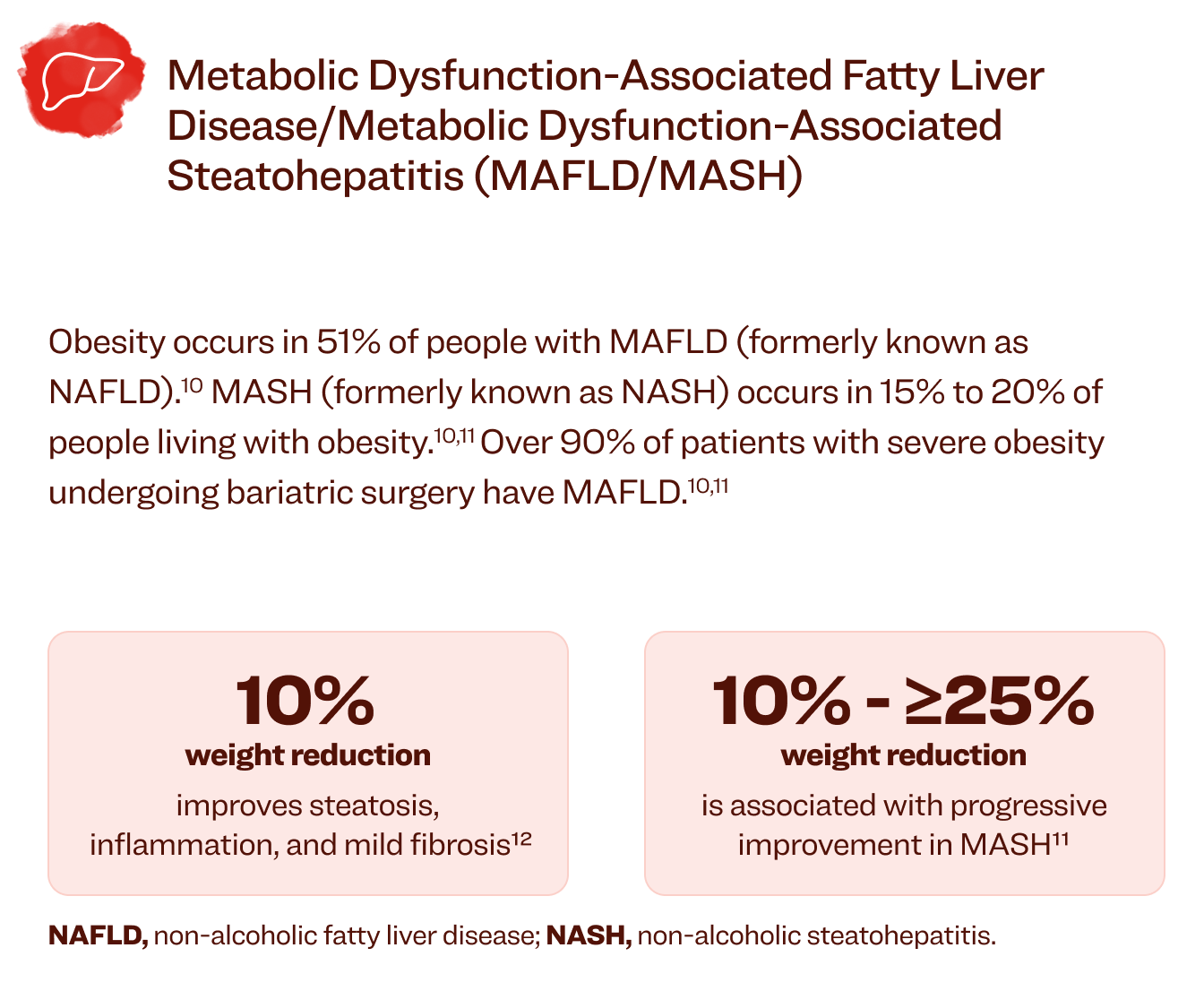
BMI, body mass index; MAFLD, metabolic dysfunction-associated fatty liver disease; MASH, metabolic dysfunction-associated steatohepatitis.
References

Obesity is a complex chronic disease that requires individualized treatment and long-term support like any other complex chronic disease2
Providing comprehensive and compassionate care to people living with obesity can lead to positive changes in obesity-related complications and improved quality of life.4
Lifestyle interventions alone are often ineffective in sustaining weight loss.5,6 Treatment modalities for obesity include lifestyle changes, psychological interventions, pharmacological management, and bariatric surgery.2


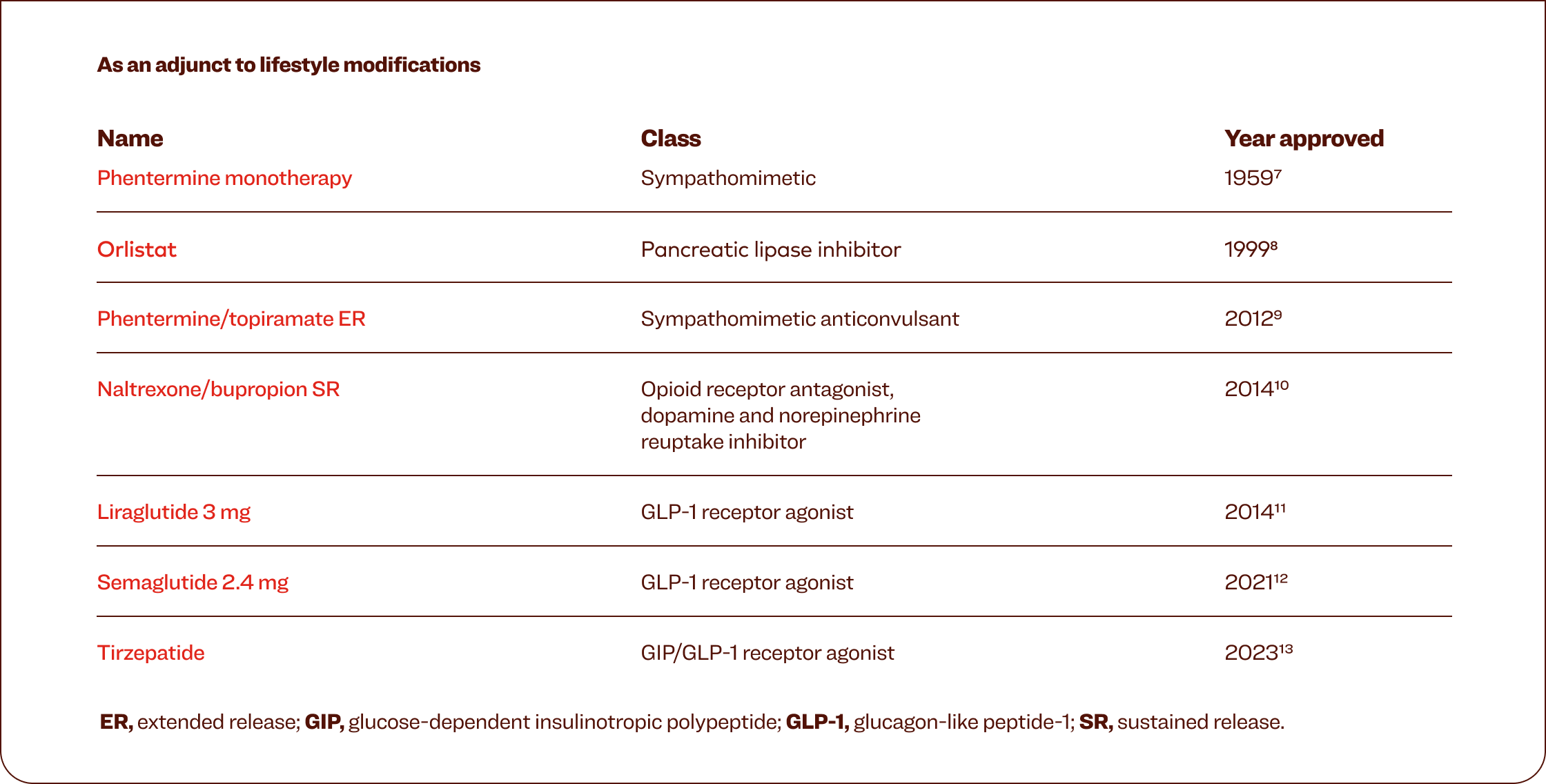
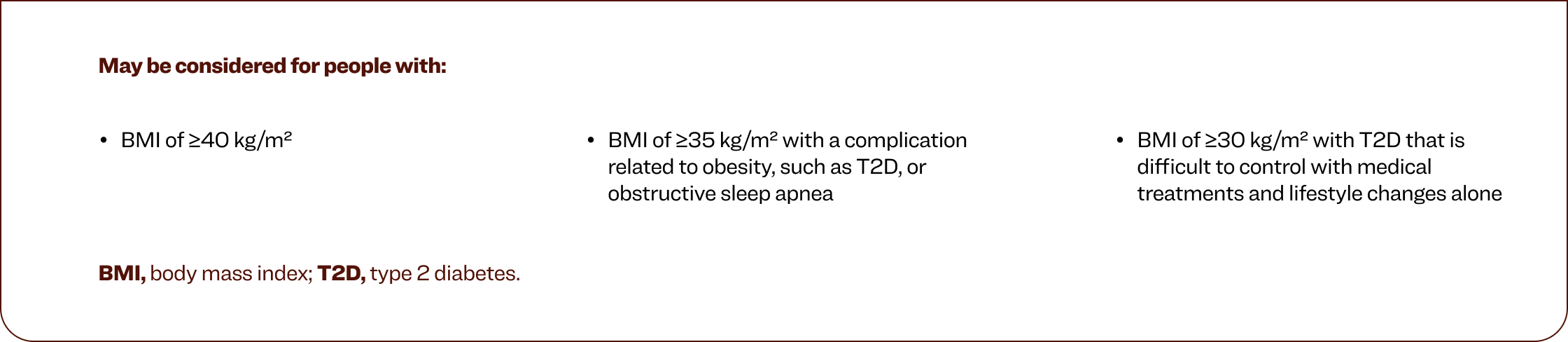
May be considered for people with:
BMI, body mass index; T2D, type 2 diabetes.
The “5 As” model can help you discuss weight management with patients14
Ask permission to discuss weight; be nonjudgmental and explore the patient’s readiness for change.
Assess body mass index, waist circumference, and obesity stage; explore drivers and complications of excess weight.
Advise the patient about the health risks of obesity, the benefits of modest weight loss, the need for long term strategy, and treatment options.
Agree on realistic weight loss expectations, targets, behavioral changes, and specific details of the treatment plan.
Assist in identifying and addressing barriers; provide resources, assist in finding and consulting with appropriate providers, and arrange regular follow ups.

for obesity, despite it being recognized by the World Obesity Federation and the
American Medical Association as a serious, chronic, relapsing disease15
References